Routine preoperative tests for elective surgery: summary of updated NICE guidance
BMJ 2016; 354 doi: https://doi.org/10.1136/bmj.i3292 (Published 14 July 2016) Cite this as: BMJ 2016;354:i3292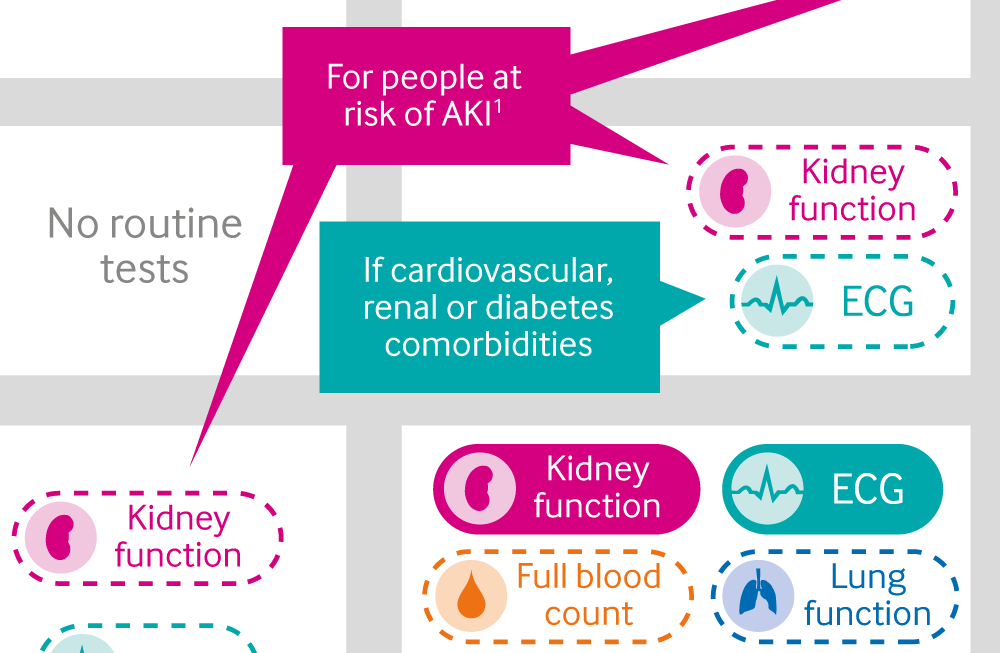
Infographic: Recommended tests before elective surgery
A visual summary of tests to offer, according to the patient's physical status and the complexity of the planned surgical procedure
- Frank O’Neill, senior research fellow1,
- Eleanor Carter, trainee specialist advisor, specialty registrar in anaesthesia1 2,
- Natalie Pink, project manager1,
- Ian Smith, chair of Guideline Development Group, senior lecturer in anaesthesia1 3
- 1National Clinical Guideline Centre
- 2Cambridge University Hospitals NHS Trust
- 3University Hospitals of North Midlands
- Correspondence to: N Pink natalie.pink{at}rcplondon.ac.uk
What you need to know
Excessive preoperative testing may cause anxiety, delays in treatment, and further unnecessary treatments without influencing outcome or changing perioperative management
Include the results of tests undertaken in primary care when referring people for surgical consultation to avoid unnecessary repetition
Patients who are relatively healthy or having relatively non-invasive surgery may require few, if any, preoperative tests
Before ordering lung function tests or an echocardiogram, consider discussing the patient with an anaesthetist
Routine preoperative investigations are expensive, labour intensive, and of questionable value, especially as they may contribute to morbidity or cause additional delays due to spurious results.1 2 3 4 5 Preoperative assessment clinics are usually based in the hospital where surgery will occur and are run according to local policies and procedures. The number of elective surgeries within the NHS has risen: 10.6 million operations took place in 2012-13 compared with 6.61 million in 2002-03. Even if only a small percentage of tests are unnecessary, large numbers of patients will be affected.
Elective surgeries are those scheduled in advance and excludes medical emergencies. The guidance covers patients over 16 years old. It includes healthy people and those who have one or more of the following comorbidities—cardiovascular, respiratory, renal, diabetes, and obesity—who are having minor, intermediate, or major or complex elective surgery (box 1). Individuals are classified by the severity of disease using the American Society of Anesthesiologists (ASA) classification system (box 2), and extent of surgery to guide testing.
Box 1: Surgery grades and examples
Minor
Excising skin lesion
Draining breast abscess
Intermediate
Primary repair of inguinal hernia
Excising varicose veins in the leg
Tonsillectomy or adenotonsillectomy
Knee arthroscopy
Major or complex
Total abdominal hysterectomy
Endoscopic resection of prostate
Lumbar discectomy
Thyroidectomy
Total joint replacement
Lung operations
Colonic resection
Radical neck dissection
There is no widely accepted and validated system for classifying the stressfulness of operative procedures, so the Guideline Development Group adopted a simple scale, illustrated with examples for the updated guidance.
Box 2: American Society of Anesthesiologists (ASA) Physical Status Classification System
This box sets out the ASA grades used in this guideline (adapted from the ASA website6)
ASA grade 1—A normal healthy person
ASA grade 2—A person with mild systemic disease
ASA grade 3—A person with severe systemic disease
ASA grade 4—A person with severe systemic disease that is a constant threat to life
The ASA classification is a simple scale describing fitness to undergo an anaesthetic. The ASA does not endorse any elaboration of these definitions, but anaesthetists in the UK often qualify (or interpret) these grades as relating to functional capacity (that is, ASA grade 2 = comorbidity that does not limit a person’s activity, ASA grade 3 = comorbidity that does limit a person’s activity).
All recommendations in this guideline were made in line with recommendations (including those on consent and capacity) from the NICE patient experience guideline.7
Changes since the 2003 guideline
Most patients are seen up to 12 weeks before surgery in a preoperative assessment clinic in the UK, where a structured history is taken and targeted examination performed by nursing staff according to protocols developed by anaesthetists11 12
Unnecessary preoperative tests, particularly in young and healthy people, have been reduced since NICE issued its guidance in 2003,13 but some continue to be ordered14
New tests such as cardiopulmonary exercise testing and polysomnography are used in preoperative assessment for patients undergoing elective surgery
In view of evidence that people with obesity and diabetes require different preoperative tests, because of the associated risk of complications during operations, separate recommendations have been made for these populations
Preoperative testing of children and of patients undergoing cardiothoracic procedures or neurosurgery is specialised, and guidance on the care of such patients has been removed from NICE guidance as it is covered elsewhere
NICE recommendations are based on systematic reviews of best available evidence and explicit consideration of cost effectiveness. However, a review of newly published material highlighted the paucity of evidence in this subject, and a modified Delphi consensus survey was undertaken to evaluate the use of most preoperative tests. In addition, the experience and opinion of the Guideline Development Group (GDG) of what constitutes good practice was used to update and replace all recommendations from the 2003 guideline.
Recommendations
See infographic for summary of preoperative tests (including blood tests) before elective surgery.
Existing test results
Ensure that the results of any preoperative tests undertaken in primary care are included when referring people for surgical consultation. [Based on GDG consensus]
Take into account any medicines people are taking when considering whether to offer any preoperative test. [Based on GDG consensus]
Other healthcare professionals or teams, or those referring for surgery, may have information of use to those carrying out preoperative assessments, such as blood tests or an electrocardiogram. Including this information at the time of referral may avoid unnecessary duplicate tests. Include tests tailored to specific comorbidities or medication that the patient is taking—for example, consider renal function testing in those taking diuretics, the latest international normalised ratio (INR), or enclosing an electrocardiogram for those with a known cardiac problem.
Pregnancy tests
The need to test for pregnancy depends on the risk presented to the woman and the fetus by the anaesthetic and the procedure.8 Anaesthesia and surgery are associated with an increased risk of spontaneous miscarriage. A systematic review found 5.8% spontaneous miscarriage in women who underwent a surgical intervention in pregnancy; 10.5% if the surgery occurred in the first trimester.9
On the day of surgery, sensitively ask all women of childbearing potential whether there is any possibility they could be pregnant. [Based on GDG consensus]
Make sure that women who could possibly be pregnant are aware of the risks of the anaesthetic and the procedure to the fetus. [Based on GDG consensus]
Document all discussions with women about whether to carry out a pregnancy test. [Based on GDG consensus]
Carry out a pregnancy test with the woman’s consent if there is any doubt about whether she could be pregnant. [Based on GDG consensus]
Develop locally agreed protocols for checking pregnancy status before surgery. [Based on GDG consensus]
Make sure protocols are documented and audited, and in line with statutory and professional guidance. [Based on GDG consensus]
Sickle cell disease or sickle cell trait tests
Sickle cell disease is of relevance to surgery. By adulthood, sickle cell disease will be clinically evident. In the absence of clinical disease, a test may discover an unknown trait, but this will not alter the patient’s management.
Do not routinely offer testing for sickle cell disease or sickle cell trait before surgery. [Based on GDG consensus]
Ask the person having surgery if they or any member of their family have sickle cell disease. [Based on GDG consensus]
If the person is known to have sickle cell disease and the disease is managed by a specialist sickle cell service, liaise with this team before surgery. [Based on GDG consensus]
HbA1c testing
HbA1c tests reflect diabetic control over the previous three months and the likely stability of glycaemic control at time of surgery.
Do not routinely offer HbA1c testing before surgery to people without diagnosed diabetes. [Based on systematic review]
People with diabetes who are referred for surgical consultation from primary care should have their most recent HbA1c test results included in their referral information. [Based on systematic review]
Offer HbA1c testing to people with diabetes having surgery if they have not been tested in the past three months. [Based on systematic review]
Urine tests
Do not routinely offer urine dipstick tests before surgery. [Based on GDG consensus]
Consider microscopy and culture of midstream urine sample before surgery if the presence of a urinary tract infection would influence the decision to operate. [Based on GDG consensus]
Chest x ray
Do not routinely offer chest x rays before surgery. [Based on GDG consensus]
Echocardiography
Do not routinely offer resting echocardiography before surgery. [Based on systematic review]
Consider resting echocardiography if the person has:
Heart murmur and any cardiac symptom (including breathlessness, pre-syncope, syncope, or chest pain) or
Signs or symptoms of heart failure.
[Based on systematic review]
Before ordering a resting echocardiogram, carry out a resting electrocardiogram and discuss the findings with an anaesthetist. [Based on systematic review]
Overcoming barriers to optimal treatment
We do not anticipate these guidelines will be associated with large change in practice.
Adopting the recommendations of the updated NICE guidance may require clinics to modify their protocols and to invest in staff training required for implementation. It is important to highlight changes from previous guidance so that staff offer tests in accordance with new guidelines. NICE has produced tools and resources to put this guideline into practice (www.nice.org.uk/guidance/ng45/resources).
Clinics will also require sufficient access to consultant anaesthetist input to adopt the NICE guidance on preoperative use of echocardiography, lung function tests, and arterial blood gases. Additional resource may be required, as anaesthetists may be consulted more frequently, but this is unlikely to be substantial. However, trusts will be required to establish or improve current mechanisms to achieve this. This is in line with national guidance on provision of anaesthetic services in the preoperative setting.10
Communication between primary and secondary care may also need improvement, to ensure all relevant test results are shared between referring primary care centres and preoperative assessment clinics. This should be carried out in accordance with the patient experience guideline.
How patients were involved in the creation of this article
Two patient representatives contributed to the development of the published recommendations as members of the Guideline Development Group. Patient organisations took part in stakeholder consultation processes during the scoping and development phases. Both of the patient representatives checked and approved the contents of this article.
Further information on the guidance
Methods
The guideline was developed using current National Institute for Health and Care Excellence (NICE) guideline methodology (www.nice.org.uk/article/PMG20/chapter/1%20Introduction%20and%20overview). The Guideline Development Group comprised three consultant anaesthetists, a consultant in clinical biochemistry and metabolic medicine, a consultant general and colorectal surgeon, a consultant physician in geriatrics and general internal medicine, a pre-assessment lead nurse, a consultant respiratory physician, a ward sister, and a consultant thoracic surgeon, alongside two lay members.
The GDG developed clinical questions, collected and appraised clinical evidence, and evaluated the cost effectiveness of proposed interventions and management strategies through literature review and economic analysis. Quality ratings of the evidence for intervention and prognostic reviews were based on GRADE methodology (www.gradeworkinggroup.org). These relate to the quality of the available evidence for assessed outcomes rather than the quality of the clinical study. As a paucity of evidence was identified within the clinical area, the GDG conducted a modified Delphi consensus survey of clinicians to inform recommendations. The survey was used to generate, analyse, and synthesise expert views to reach a group consensus position. The GDG reviewed the results of the survey, in addition to the clinical evidence and their own experience, to produce the guideline.
The draft guideline went through a rigorous review process, in which stakeholder organisations were invited to comment; the GDG took all comments into consideration when producing the final version of the guideline.
NICE has produced three versions of the guidance: a full version (www.nice.org.uk/guidance/ng45/evidence); a summary version known as the “NICE guidance” (www.nice.org.uk/guidance/ng45); and a version for people using NHS services, their families and carers, and the public (www.nice.org.uk/guidance/NG45/ifp/chapter/about-this-information). These versions, as well as a pathway, are available from the NICE website (http://pathways.nice.org.uk/pathways/preoperative-tests). Updates of the guideline will be produced as part of NICE’s guideline development programme.
Further research
Polysomnography
Does preoperative screening of people who are at risk of obstructive sleep apnoea (OSA) with polysomnography identify those at higher risk of postoperative complications?
Does treating OSA perioperatively improve outcomes?
Perioperative management of HbA1c
Does optimisation of HbA1c in people with poorly controlled diabetes improve surgical outcomes?
Footnotes
Contributors: All authors contributed to the conception and drafting of this article, and to revising it critically. They have all approved this version. FON is guarantor.
Funding: FON and NP are employees of the National Clinical Guideline Centre, at the Royal College of Physicians, which is commissioned and funded by NICE to develop clinical guidelines.
Competing interests: We declare no competing interests, based on NICE's policy on conflicts of interests (available at www.nice.org.uk/Media/Default/About/Who-we-are/Policies-and-procedures/code-of-practice-for-declaring-and-managing-conflicts-of-interest.pdf). The guidance authors’ full statements can be viewed at www.nice.org.uk/guidance/ng45/evidence/appendix-b-declarations-of-interest-2423837487.
